Overview / Definition
Azoospermia is a condition found in approximately 1% of all males. Evaluation of this condition is defined after a qualified search confirming the absence of sperm cells in two separate semen samples. A true diagnosis of azoospermia requires a comprehensive study of the patient’s full medical history, in addition to a physical examination and full battery of endocrine testing.
Azoospermia is usually divided into two categories: Obstructive azoospermia (OA) and non-obstructive azoospermia (NOA).
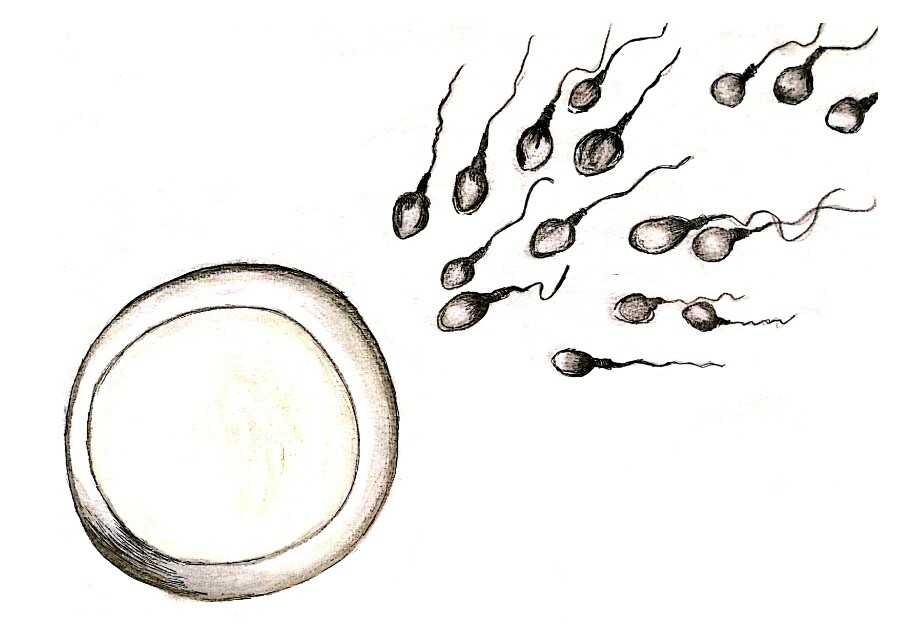
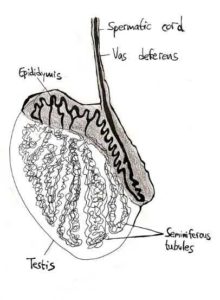
Normal development of sperm cells, known as spermatogenesis, takes place in the testes. From there the mature sperm then progress through the vas deferens onward through the urethral canal and are discharged from the penis.)
Detailed / Azoospermia type explained and determined
The division of azoospermia into two categories is based on where in spermatogenesis the problem occurs.
A diagnosis of obstructive azoospermia (OA) indicates a post-testicular cause, where the sperm has successfully matured however is unable to reach the ejaculate.
Non-obstructive azoospermia (NOA) indicates a failure at some point during spermatogenesis in the testes, in which case mature sperm are not produced and will, therefore, be absent in the ejaculate.
Several methods are employed to differentiate between obstructive and non-obstructive azoospermia.
When the volume of the semen sample is low, it is a likely indication of an ejaculatory duct obstruction (ie OA). This diagnosis can be further verified by a low semen acidity and absent levels of fructose in the sample. In these patients, testosterone levels may be normal.
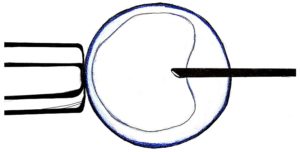
Here, it is possible that the culprit may be retrograde ejaculation–a process where the semen is ejaculated via the urethra, becoming redirected to the bladder as opposed to the penis. A post-ejaculate urinalysis (PEU, also known as a PEUT) can be used to verify such a case, in which the urinalysis would indicate millions of sperm.
If the PEU does not reveal the presence of sperm in the urine, a transrectal ultrasound can evaluate enlargement of the seminal vesicles or the ejaculatory ducts, as well as identify midline cysts, in an attempt to pinpoint the cause of the obstruction.
Patients with OA will usually have normal levels of FSH (a hormone that stimulates spermatogenesis), normal testicular volume, and palpable vasa.
In contrast, azoospermic men who present with small testes and high FSH levels indicate a non-obstructive cause, where failure to develop the sperm cells to maturity may occur at various points along with the development. These samples will have both normal semen volume and acidity.
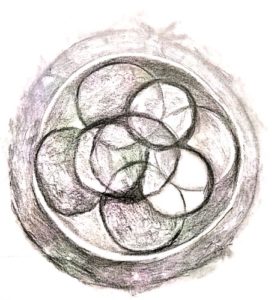
An NOA diagnosis can be confirmed with a testicular biopsy, which will reveal abnormal cell patterns, maturation arrest of the spermatogonia, or hypospermatogenesis.
While it was once thought that males diagnosed with NOA did not have any sperm, more recent advances in surgical and analysis techniques have to lead to a slow increase in the number of patients where testicular biopsy or TESE reveal a sufficient number of mature sperm cells. These sperm cells may then be used for intracytoplasmic sperm injection (ICSI) during in vitro fertilization (IVF).